Terapia obwodowa Multispot
Fotokoagulacja panretinalna (PRP) pozostaje standardem opieki w zaawansowanej retinopatii cukrzycowej (DR) od późnych lat 70., gdy dane z badań Diabetic Retinopathy Study (DRS) i Early Treatment Diabetic Retinopathy Study (ETDRS) [1, 2] dowiodły korzyści z takiego postępowania w profilaktyce utraty wzroku na etapach proliferacyjnych tej choroby.
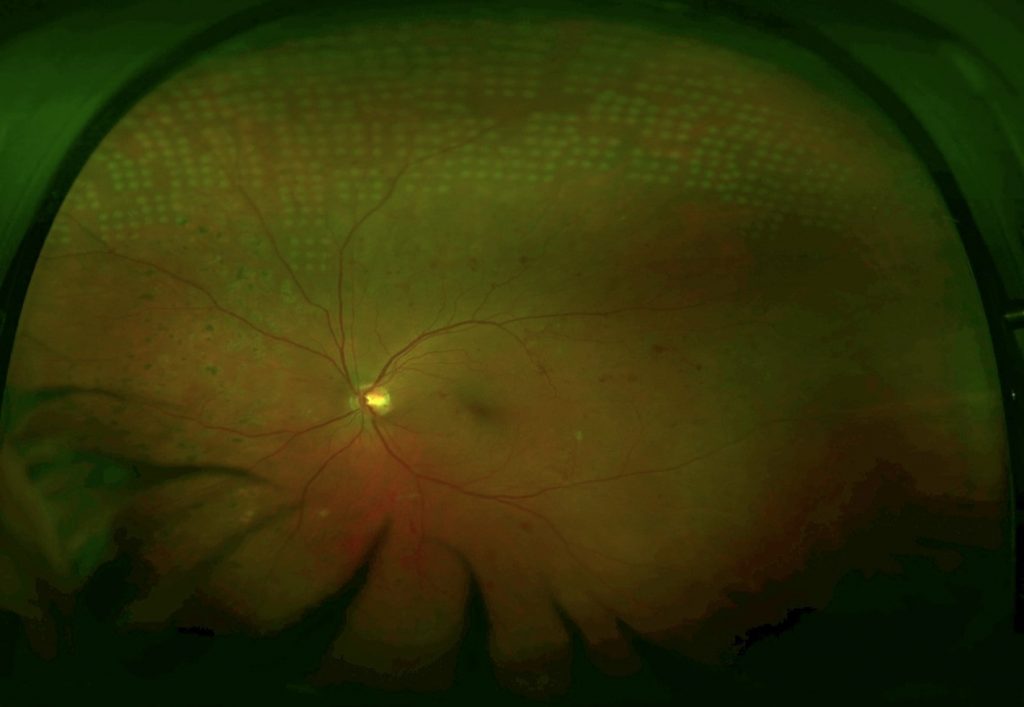
Konwencjonalna PRP Single Spot z zasady powoduje uszkodzenie, jednak w ostatnim dziesięcioleciu wprowadzono nowe technologie, dzięki czemu opracowano nowe generacje systemów laserów: lasery MultiSpot. Umożliwiają one wygenerowanie pojedynczego impulsu laserowego, krótszego o cały rząd wielkości (0,01–0,02 s). Te impulsy są wysyłane w szybkich sekwencjach jeden po drugim, tworząc tzw. wzorce.
Wytyczne dotyczące leczenia
Fotokoagulacja laserem MultiSpot jest innowacyjną metodą dostarczania energii laserowej do siatkówki.
Przed rozpoczęciem laseroterapii należy precyzyjnie dostosować energię laserową wymaganą do uzyskania pojedynczego punktu wiązki laserowej (przy krótszej długości impulsu).
Dane kliniczne
Tryb leczenia MultiSpot, w którym stosuje się krótkie impulsy (od 10 do 20 ms), ma pod wieloma względami przewagę nad konwencjonalną fotokoagulacją siatkówki, np. fotokoagulacją panretinalną (PRP):
- Jako, że mniej ciepła rozprzestrzenia się do siatkówki i naczyniówki, dochodzi do mniejszych uszkodzeń warstwy włókien nerwowych siatkówki1,2
- Terapia jest bardziej komfortowa i lepiej tolerowana przez pacjentów3
- Czas terapii jest krótszy (całkowitą PRP osiąga się po 1 sesji) 4
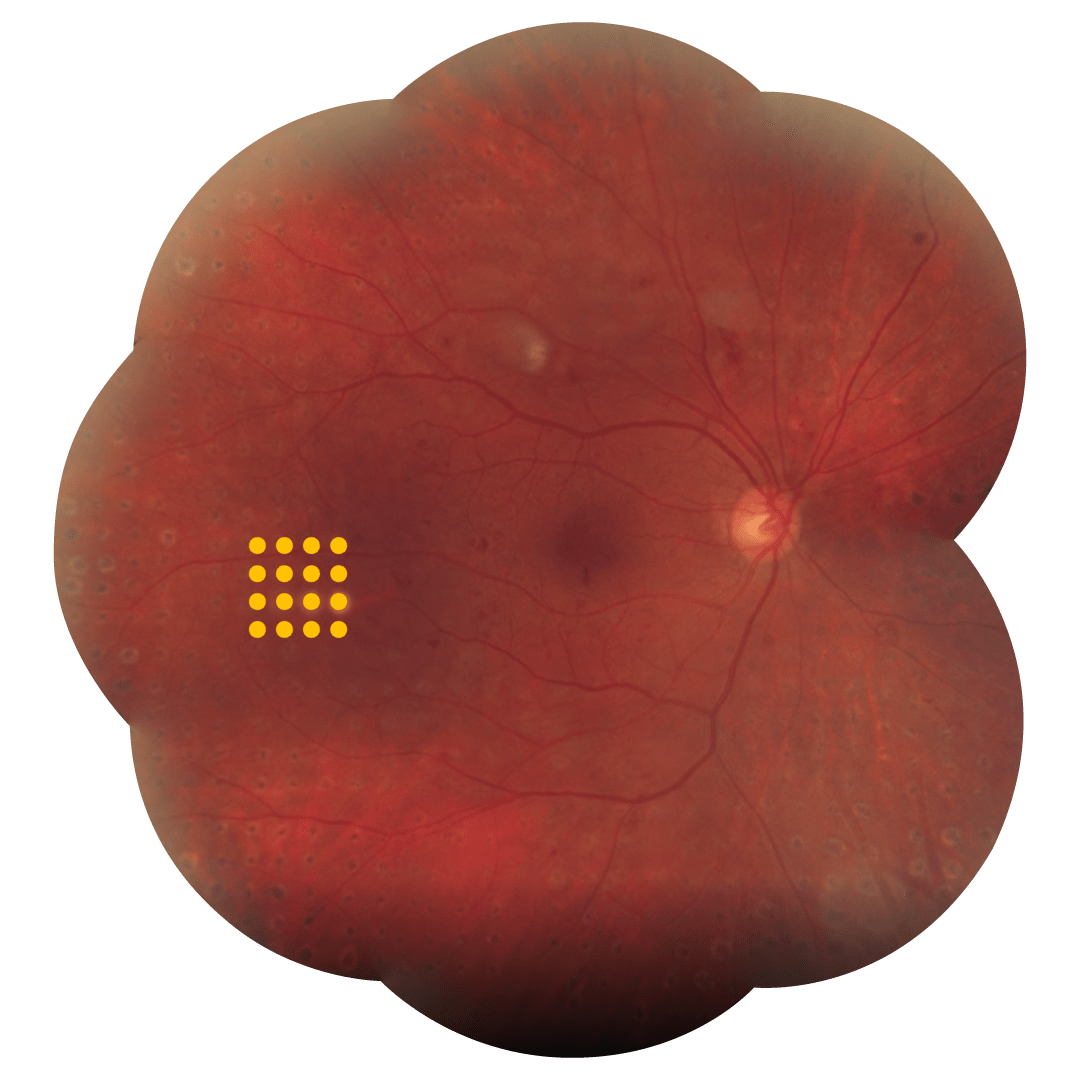
Tryb leczenia MultiSpot można wybrać spośród 4 spersonalizowanych wzorców przeprowadzania terapii, aby lepiej dopasować ją do miejsca leczonego: kwadraty, koła, potrójny łuk, pojedynczy punkt.
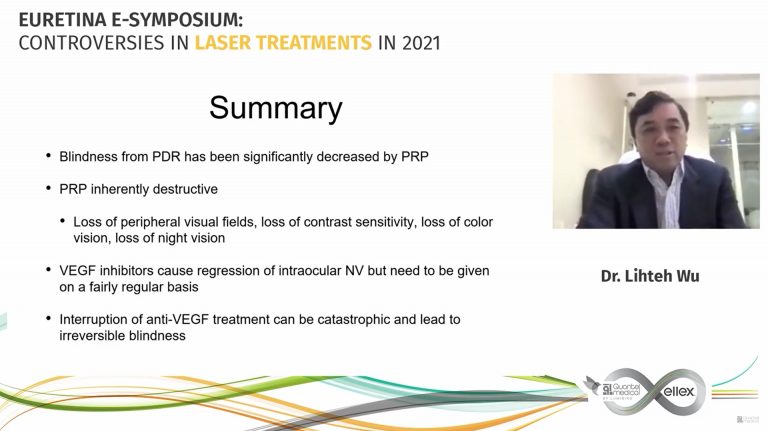
Anti-VEGF vs Laser for PDR, a changing treatment paradigm?




Lekarze
Porozmawiaj o Wielopunktowej
terapii laserowej
Bibliografia
Objective: To systematically evaluate the effects of laser beam size, power, and pulse duration of 1 to 100 milliseconds on the characteristics of ophthalmoscopically visible retinal coagulation lesions.
Methods: A 532-nm Nd:YAG laser was used to irradiate 36 retinas in Dutch Belt rabbits with retinal beam sizes of 66, 132, and 330 mum. Lesions were clinically graded 1 minute after placement, their size measured by digital imaging, and their depth assessed histologically at different time points.
Results: Retinal lesion size increased linearly with laser power and logarithmically with pulse duration. The width of the therapeutic window, defined by the ratio of the threshold power for producing a rupture to that of a mild coagulation, decreased with decreasing pulse durations. For 132- and 330-mum retinal beam sizes, the therapeutic window declined from 3.9 to 3.0 and 5.4 to 3.7, respectively, as pulse duration decreased from 100 to 20 ms. At pulse durations of 1 millisecond, the therapeutic window decreased to unity, at which point rupture and a mild lesion were equally likely to occur.
Conclusions: At shorter pulse durations, the width and axial extent of the retinal lesions are smaller and less dependent on variations in laser power than at longer durations. The width of the therapeutic window, a measure of relative safety, increases with the beam size.
Clinical relevance: Pulse durations of approximately 20 milliseconds represent an optimal compromise between the favorable impact of speed, higher spatial localization, and reduced collateral damage on one hand, and sufficient width of the therapeutic window (> 3) on the other.
Purpose
To examine the effects of panretinal photocoagulation (PRP) using a pattern scanning laser (PASCAL) system on the retinal nerve fiber layer (RNFL) thickness in patients with diabetic retinopathy.
Methods
This retrospective study included 105 eyes with diabetic retinopathy, which consisted of three groups: the PASCAL group that underwent PRP with the PASCAL method (33 eyes), the conventional group that underwent conventional PRP treatment (34 eyes), and the control group that did not receive PRP (38 eyes). The peripapillary RNFL thickness was measured by optical coherence tomography before, six months, and one year after PRP to evaluate the changes in peripapillary RNFL.
Results
The RNFL thickness in the PASCAL group did not show a significant difference after six months (average 3.7 times, p = 0.15) or one year after the PRP (average 3.7 times, p = 0.086), whereas that in the conventional group decreased significantly after six months (average 3.4 times, p < 0.001) and one year after PRP (average 3.4 times, p < 0.001).
Conclusions
The results of this study suggest that the PASCAL system may protect against RNFL loss by using less energy than conventional PRP.
Purpose: We performed a study of laser panretinal photocoagulation in 20 patients with proliferative retinopathy. We compared short exposure, high-energy laser settings with conventional settings, using a 532 nm, frequency doubled, Neodymium-Yag laser and assessed the patients in terms of pain experienced and effectiveness of treatment.
Methods: Twenty patients having panretinal photocoagulation for the first time underwent random allocation to treatment of the superior and inferior hemi-retina. Treatment A used 'conventional’ parameters: exposure time 0.1 s, power sufficient to produce a visible grey-white burns, spot size 300 microm. The other hemi- retina was treated with treatment B using exposure 0.02 s, 300 microm and sufficient power to have similar endpoint. All patients were asked to evaluate severity of pain on a visual analogue scale. (0=no pain, 10=most severe pain). All patients were masked as to the type of treatment and the order of carrying out the treatment on each patient was randomised. Patients underwent fundus photography and were followed up for 6-45 months.
Results: Seventeen patients had proliferative diabetic retinopathy, two had ischaemic central retinal vein occlusion and one had ocular ischaemic syndrome. The mean response to treatment A was 5.11, compared to 1.40 treatment B, on the visual analogue scale, which was statistically significant (P=0.001). All patients preferred treatment B. Further treatments, if required, were performed with treatment B parameters and long-term follow-up has shown no evidence of undertreatment.
Conclusions: Shortening exposure time of retinal laser is significantly less painful but equally effective as conventional parameters.
Objective: To investigate the effects of pattern scanning laser (Pascal; OptiMedica, Santa Clara, California) multispot panretinal photocoagulation given in a single-session (SS-PRP) vs single-spot multiple-session PRP (MS-PRP) on proliferative diabetic retinopathy (PDR).
Methods: Single-center, randomized clinical trial of 40 eyes. Proliferative diabetic retinopathy was treated with a 400-mum spot size in 1500 burns given either as Pascal in 20-millisecond SS-PRP or in 3 sessions (100-millisecond MS-PRP) during a 4-week period. Visual acuity, central subfield retinal thickness (CRT), and 24-2 Swedish interactive thresholding algorithm visual fields were recorded at baseline and 4 and 12 weeks.
Main outcome measures: Central subfield retinal thickness, mean deviation, and PDR grade at 12 weeks.
Results: There was a significant increase in mean CRT with MS-PRP (22 mum at 4 weeks, 95% CI, -32.25 to -10.75; 20 mum at 12 weeks, 95% CI, -28.75 to -10.82; P < .001) and no significant increase in the SS-PRP group. The mean deviation increased significantly in the SS-PRP group after 4 weeks (0.73 dB, P = .048), with no significant changes in either group at other points. A positive effect on PDR was observed in 74% of eyes in the SS-PRP group vs 53% in the MS-PRP group (P = .31). Mean treatment time for SS-PRP was 5.04 minutes (SD, 1.5 minutes) compared with 59.3 (SD, 12.7 minutes) in the MS-PRP group (P < .001).
Conclusions: There were no adverse outcomes (CRT, visual acuity, or visual field) from using multispot SS-PRP vs single-spot MS-PRP at 12 weeks postlaser, and treatment times were significantly shorter for multispot SS-PRP. Pascal SS-PRP was as effective as MS-PRP in the treatment of PDR.
Application to clinical practice: Twenty-millisecond Pascal SS-PRP may be safely and rapidly performed in 1500 burns with a similar efficacy to conventional MS-PRP. TRIAL IDENTIFIER: Research and Development Office PIN R00037, Central Manchester University Hospitals Foundation Trust.
