A little bit of history...
In the early 1900s, Albert Einstein conceptualized the theory of “light amplification through stimulated emission of radiation”, a concept he named laser theory. For five decades, physicists and scientists continued to develop laser theory and in 1960 the very first laser was built.
In the mid-60’s, laser technology was adopted by medical professionals who believed laser light held the power to induce positive changes at the cellular level.
Thanks to the DRS and ETDRS clinical studies, laser photocoagulation has been the mainstay of diabetic retinopathy treatment since its development. With the advent of anti-VEGF therapy, the role of laser therapy appeared to be diminished, however many advances in laser technology have been developed since. From thermal laser therapy to subthreshold laser therapy.
The very beginning
Another important time
The third important time
What is Subliminal Laser Therapy?
Raison d’être: Eliminate iatrogenic damage from conventional macular photocoagulation
Subliminal laser is an alternative to the conventional continuous-wave laser for the treatment of retinal or macular diseases. In contrast to the conventional laser, the therapeutic effect of the subthreshold laser is not accompanied by thermal retinal damage. This fact is of particular importance when a treatment near the fovea is required.
This laser method has been proven to be a safe and effective treatment option for macular pathologies such as central serous chorioretinopathy (CSC), diabetic macular edema (DME).
Which wavelength?
Photocoagulation relies on the absorption of light by various ocular pigments.
The three major ocular pigments are melanin, hemoglobin and xanthophyll, which have varying affinities for different wavelengths and occur in varying proportions throughout the retina.
Theoretically, the 577-nm yellow laser light provides peak absorption of oxyhemoglobin, excellent lesion visibility, low intraocular light scattering and pain, and negligible xanthophyll absorption1,2.
The yellow 577nm wavelength has been described in bibliography as the most versatile and safe wavelength3.
Thanks to its absorption characteristics, it causes lesser scatter and requires the use of a lower energy level compared to green (532nm) and other yellow (561 to 568nm) wavelengths3.
It is minimally absorbed by macular xanthophylls45, potentially allowing for treatments close to the fovea6.
It is highly absorbed by the oxyhemoglobin (absorption peak) and thus optimal for the treatment of vascular lesions and subretinal vascular proliferations7.
What technology is used for Subliminal Laser Therapy?
SubLiminal laser therapy is a modern subthreshold laser treatment option that employs a customizable pattern grid selection and delivers treatment through a succession of short, microsecond-long pulses of laser.
This allows for cooling of the retinal pigment epithelium (RPE) between pulses, preventing a critical amount of heat from accumulating in the tissue and the consequential RPE and retinal scarring which we know to be unnecessary to attain a therapeutic response4 and to limit the possibilities for future retreatments.
Clinical data
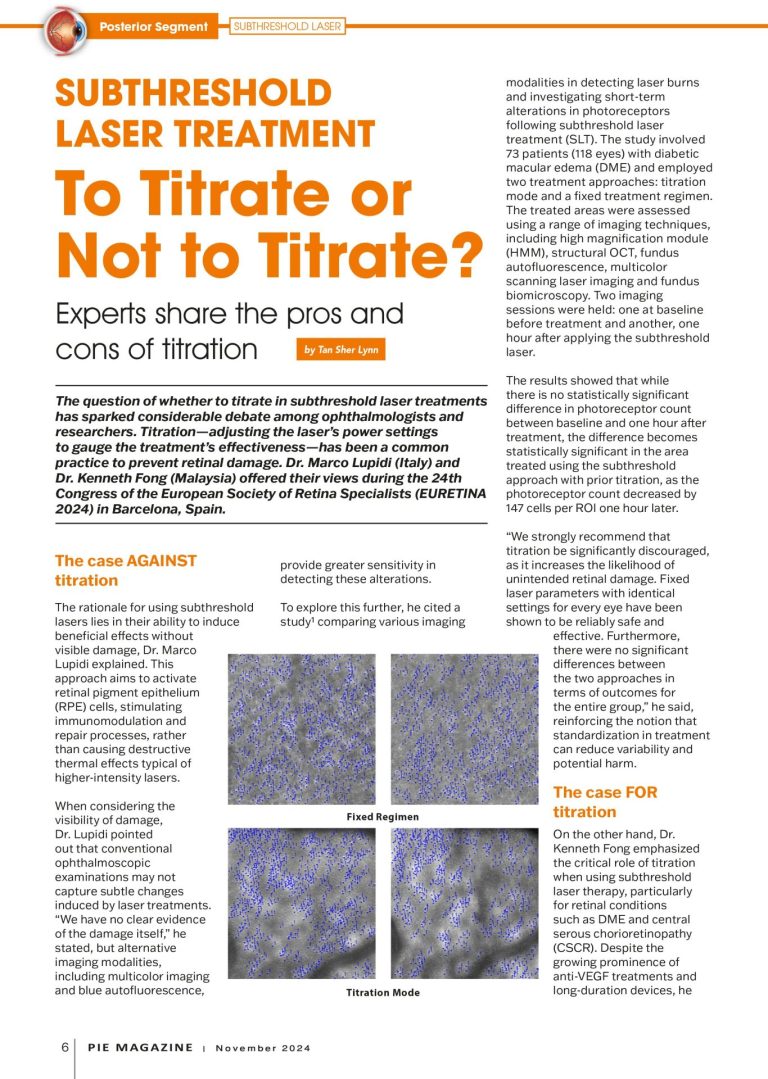
Subthreshold laser treatment: To Titrate or Not to Titrate?
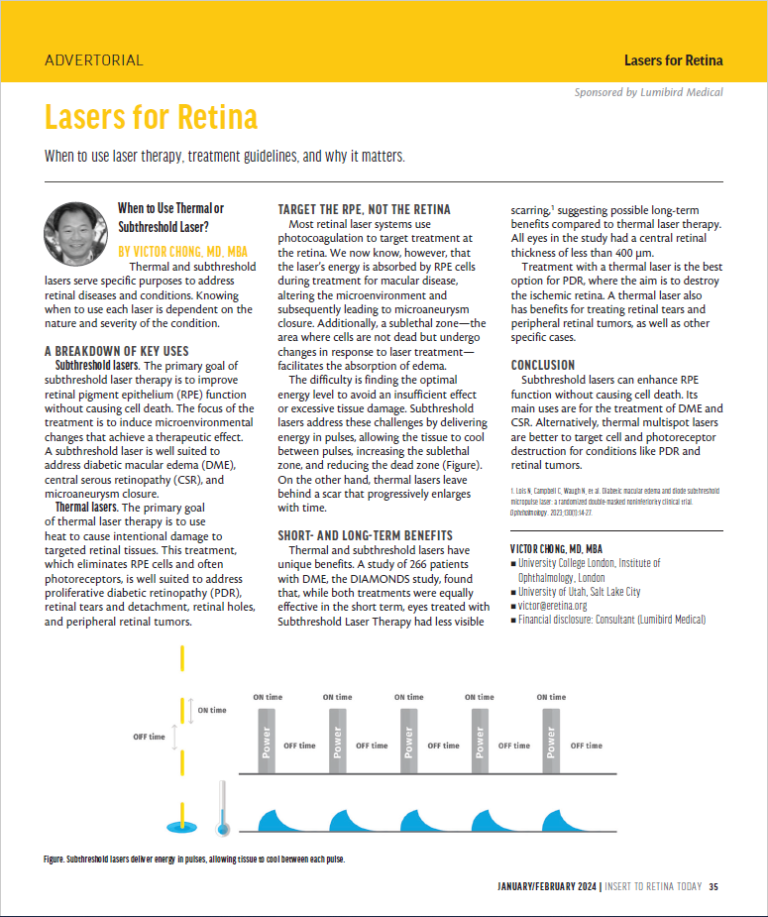
Lasers for Retina
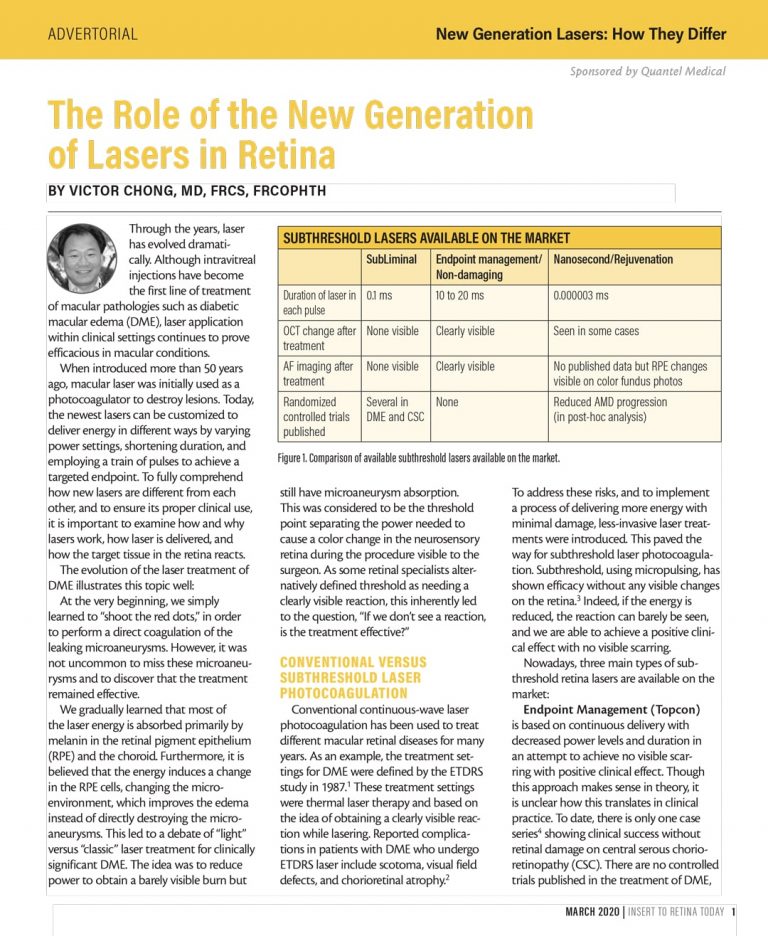
The Role of the New Generation of Lasers in Retina
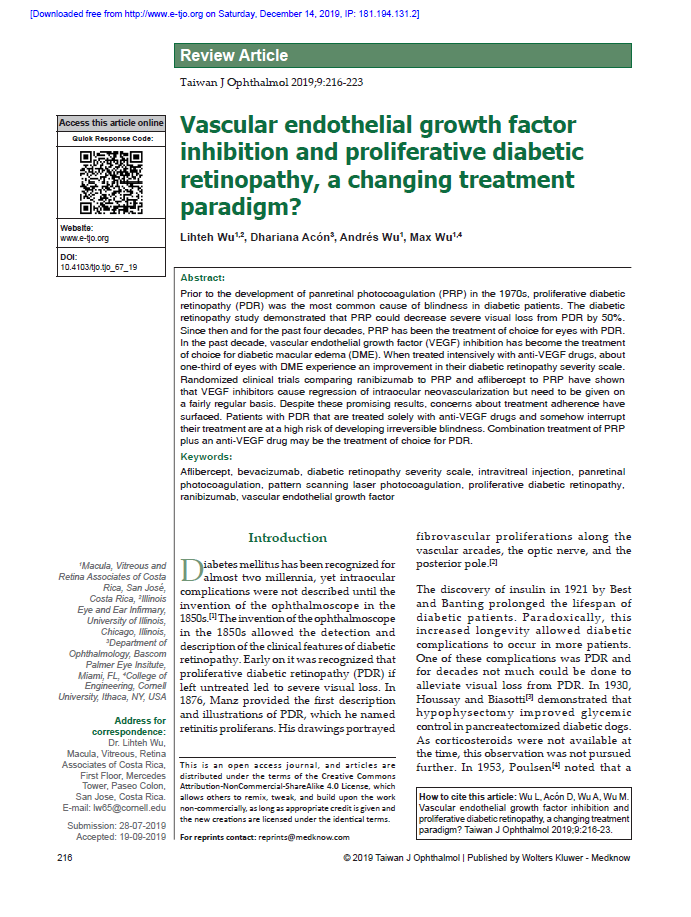
Vascular endothelial growth factor inhibition and proliferative diabetic retinopathy, a changing treatment paradigm?

How new generation lasers are different from each other
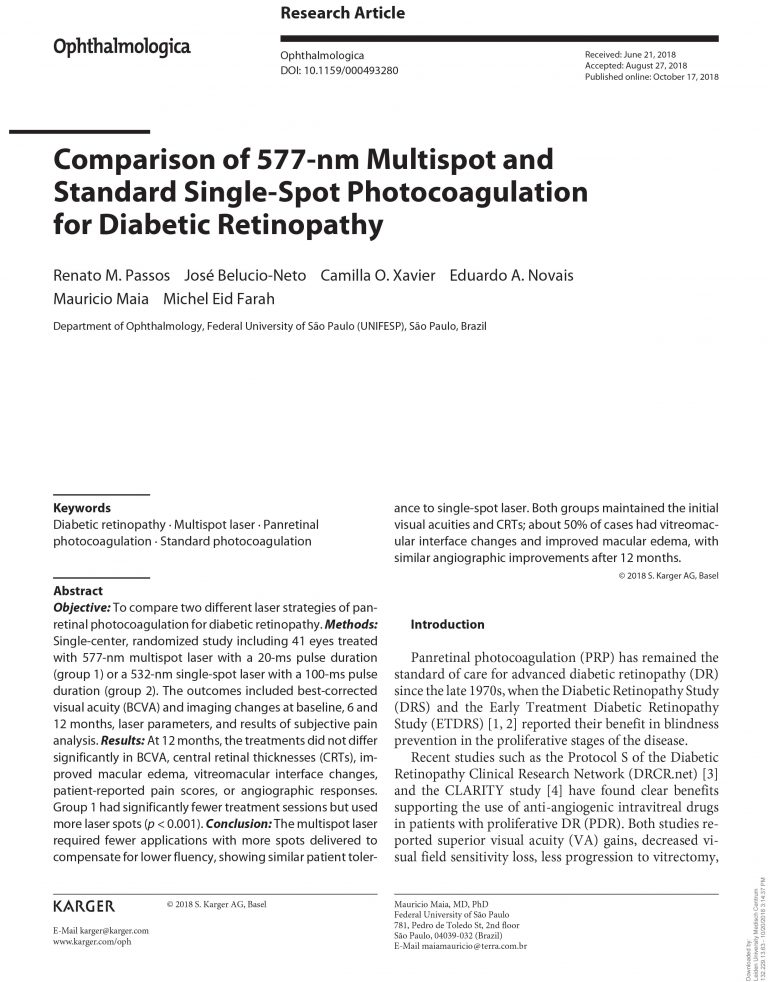
Comparison of 577-nm Multispot and Standard Single-Spot Photocoagulation for Diabetic Retinopathy
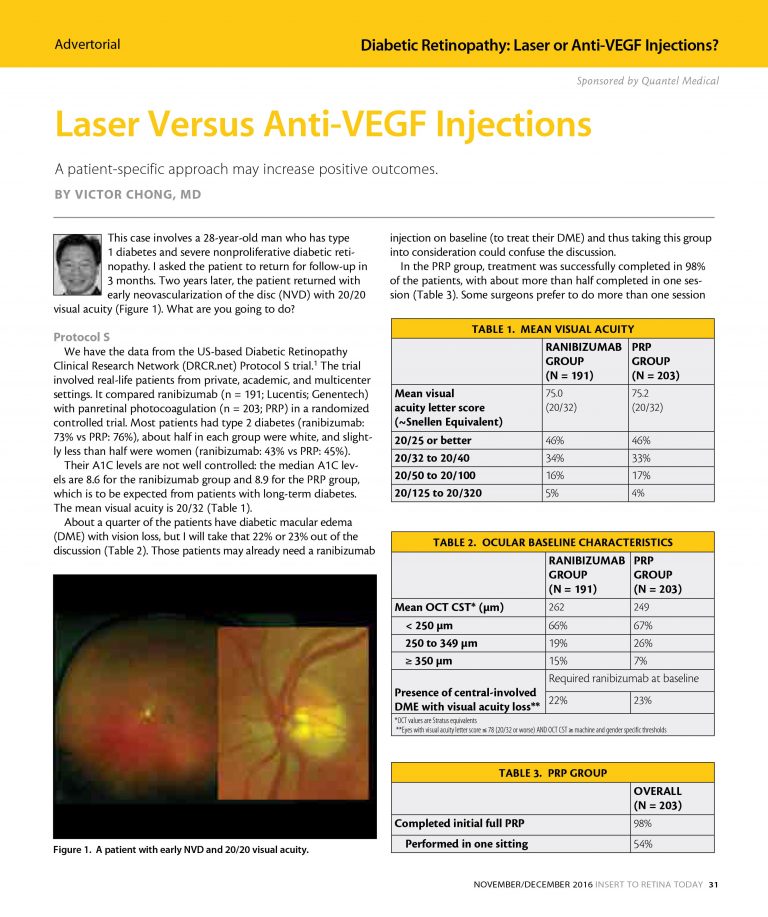
Laser Versus Anti-VEGF Injections
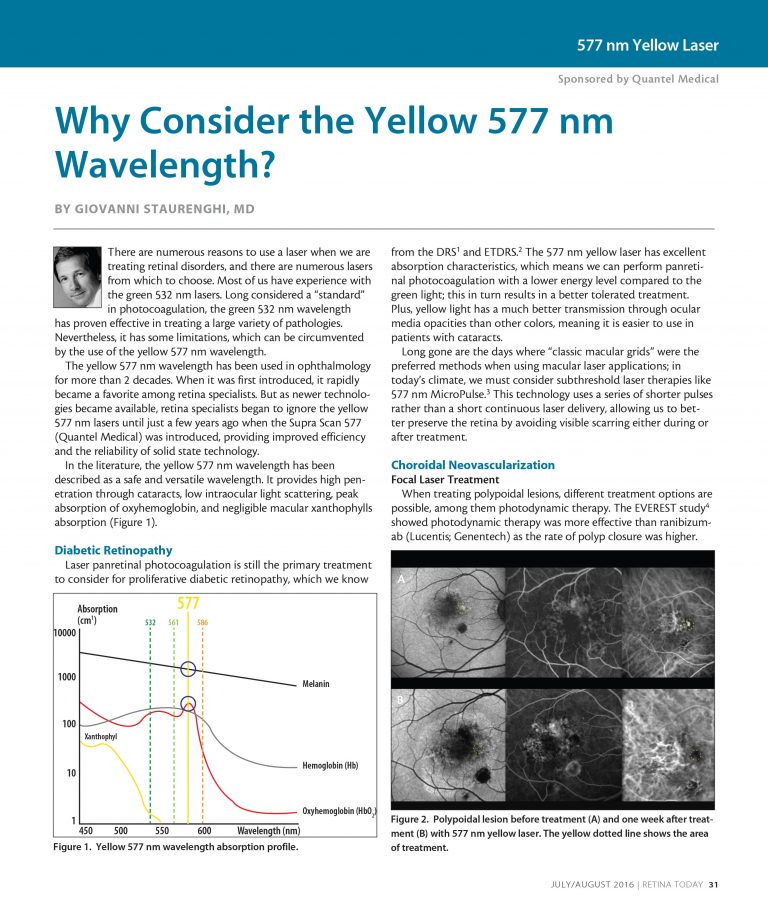
Why Consider the Yellow 577 nm Wavelength?
Clinical experience with Multispot yellow 577nm laser
A histological comparison of micropulse and standard laser treatment in threshold and sub-threshold modes

Do We Still Need Subthreshold Laser for Macular Diseases?

How to optimize retina laser treatments in 2020?
Subliminal laser treatment for macular diseases
How are retina lasers different from each other ?
Controversies on Modern Laser Treatments for Retina and Vitreous
SubLiminal Laser Therapy: Concept and reasons
Expanding clinical application of SubLiminal laser
Why consider the yellow 577nm wavelength?
Bibliography
Graefes Arch Clin Exp Ophthalmol. 1989;227:277-280.
Ophthalmology.1986;93:952-958
Purpose: This pilot study aimed to evaluate the efficacy and safety of subthreshold micropulse yellow (577-nm) laser photocoagulation (SMYLP) in the treatment of diabetic macular edema (DME).
Methods: We reviewed 14 eyes of 12 patients with DME who underwent SMYLP with a 15% duty cycle at an energy level immediately below that of the test burn. The laser exposure time was 20 ms and the spot diameter was 100 µm. Laser pulses were administered in a confluent, repetitive manner with a 3 × 3 pattern mode.
Results: The mean follow-up time was 7.9 ± 1.6 months. The baseline-corrected visual acuity was 0.51 ± 0.42 logarithm of the minimum angle of resolution (logMAR), which was improved to 0.40 ± 0.35 logMAR (p = 0.025) at the final follow-up. The central macular thickness at baseline was 385.0 ± 111.0 µm; this value changed to 327.0 ± 87.7 µm (p = 0.055) at the final follow-up.
Conclusions: SMYLP showed short-term efficacy in the treatment of DME and did not result in retinal damage. However, prospective, comparative studies are needed to better evaluate the efficacy and safety of this treatment.
Keywords: Diabetic retinopathy; Laser therapy; Macular edema.
J Ophthalmol. 2015.